
‘Knocked down hip’ is a common name for a fracture of the tuber coxae (point of hip). This is usually the result of a horse having an impact with a gate post, fence or trees, a barrel in a race, another horse’s hoof, or the ground.
A piece of bone is often completely displaced, disappearing downwards and forwards into the paralumbar fossa – the space between the transverse processes of the lumbar vertebrae, internal abdominal oblique muscle, and the last rib.
This displacement can then change the outline of the pelvis on the damaged side. That said, it isn’t always visually obvious, and many horse owners often don’t even know it has happened.
It’s the least damaging of pelvic fractures as it doesn’t involve a joint or compromise the pelvic structure, and for this reason it’s often said that its long term effects are purely cosmetic.
But does that really mean it has no lasting effects whatsoever?
This post presents a range of potential issues, from none whatsoever to an altered gait that affects performance, and explains why you should always thoroughly assess your horse for effects after a tuber coxae fracture.
(c) Jane Clothier, thehorsesback.com. With thanks to Dr Sharon May-Davis for checking this post and catching my errors.
The elusive nature of the problem
I know a horse whose owner reported a succession of minor come-and-go issues in the hindlimb.
These either failed to warrant veterinary attention (there being no lameness) and with no diagnoses made when a vet was consulted. The problem was intermittent and elusive.

There was no visible asymmetry and no muscle atrophy.
However, the horse was outwardly rotating the right stifle and swinging the leg outwards in the forwards (cranial) phase of the stride.
When I palpated the right tuber coxae, it had a section knocked away halfway up the bone.
Could there be a connection? Very likely!
Let’s take a closer look at the tuber coxae and how a fracture can affect the action of the hind limb on that side.
Why is the knocked down hip so common?
Besides being the widest point of the pelvis and therefore vulnerable to traumatic injuries of all varieties, the horse’s point of hip has another key weakness.
It’s part of a growth plate. It’s an epiphyseal plate, which means it’s separated from the main body of the pelvis by a physis, the line where bone is produced during growth in early life.
This means we’re looking at the ‘cap’ of the tuber coxae, which is a weaker cap of bone until at least 5 years of age, and often later depending on the breed.
These are vulnerable to getting displaced – the growth plate of the elbow (ulna) being another example.
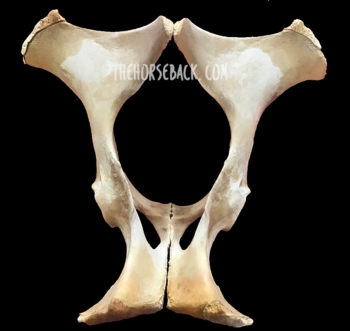
Skeletal specimens such as the one in the image show us that even beyond 5 years of age, the growth plate may not be fully attached and is a weaker structure. The tuber coxae in the mature horse still has a roughened surface due to muscle attachments, which gives it a rather open honeycomb structure. This makes it far easier to damage.
More than a cosmetic feature
The clue as to why this fracture can be damaging, even though it doesn’t affect the structural integrity of the pelvis, lies in its function.
Yes, its function. Even though it’s not a moving part, the tuber coxae is much more than a cosmetic feature. Like the withers and the elbow/ulna, its function is to provide an anchor for some important muscles.
It serves as the attachment point for muscles involved in flexing the hip and extending the stifle to move the entire hindlimb forwards (more on those later). For this reason, the attachment point needs to be extremely stable.

The tuber coxae must serve as an anchor point in this way while powerful propulsive forces are conveyed via the pelvis to the spine.
That’s why the tuber coxae are tuberosities – they sit wide and proud and, like handlebars on a motorbike, remain relatively stable in spite of the forces being transmitted from the hind legs forward along the spine.
The location of the fracture
Although generally similar, tuber coxae vary in shape from horse to horse. Fortunately, as they come in matching pairs, it’s possible to identify damage by comparing one side to the other.
Visually, it can be easy to spot a horse with an old tuber coxae fracture due to its pelvic asymmetry. How visible generally depends on the fracture’s severity.
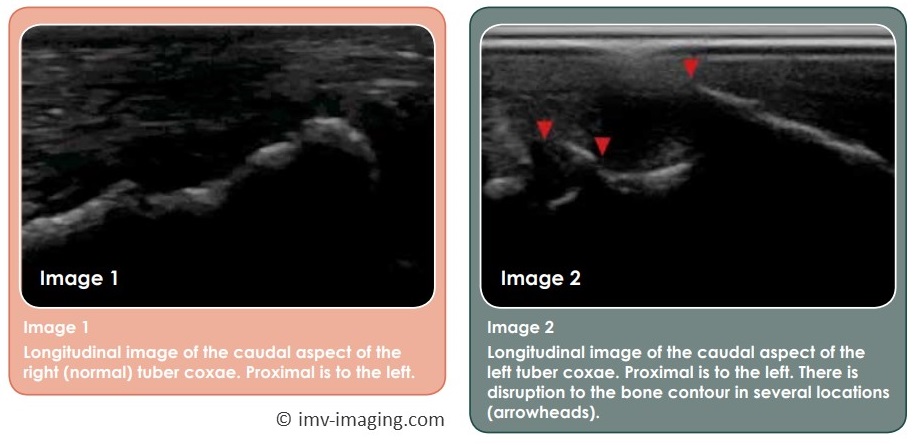
Alternatively, good old manual palpation can reveal its presence.
Here are the main possibilities.
-
Upper piece of bone is displaced

The upper part of the tuber coxae (ie. dorsomedial aspect) may be chipped off. This is usually, but not always, a visible type of fracture, as the point of hip acquires a rounded appearance. This is generally what gives the knocked down hip its name.
-
Central piece of bone is displaced

In this case, both ends of the tuber coxae are intact, so the overall shape isn’t much different.
However, if you palpate carefully, there’s a divot in the middle where a chip of bone has been dislodged. Identifying this involves comparing both sides of the horse.
-
Lower piece of bone is displaced

Only the lower part of the bone (ie. ventrolateral aspect) may be missing.
This is harder to see, but easy to feel: the tuber coxae’s ‘ledge’ is noticeably shorter.
This variation of the fracture is common as it’s the outer corner, the widest point, that’s been knocked off.
One study of 29 horses reported that when only the lower, outer aspect of the bone (caudolateral) was fractured, injured horses returned to work in around 3.5 months. [1]
-
Whole tuber coxae is displaced

In severe cases, the entire tuber coxae is displaced. The visual asymmetry is more obvious. It can also be more serious: with palpation, it may be possible to feel the wider, deeper section of bone remaining, where the ilial shaft becomes the ilial wing.
In the study, when the entire tuber coxae was fractured, the recovery period was longer at around 6.5 months from injury. [1]
Could there be more damage?
If the horse has fallen hard enough to fracture the tuber coxae, it may have damaged other areas of its pelvis too. The various sacroiliac ligaments are prime contenders, as is the sacroiliac joint itself, along with the lumbosacral joint.
Then there are the structures of the actual hip joint (acetabulum and coxofemoral) and head of the femur.
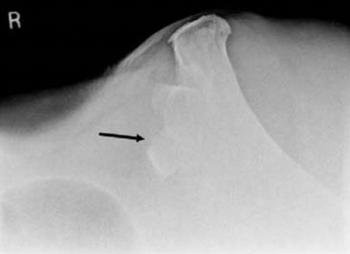
There may even be an incomplete fracture of the ilium that we don’t know about, or separation at the pelvic/pubic symphysis. A full veterinary assessment should always be sought if your horse is lame and you suspect a trauma. Radiographs, ultrasound and scintigraphy have been used to image the tuber coxae and identify the extent of the damage. [2]

On a more superficial level, a ridge of what feels like soft tissue can sometimes be moved over the remaining tuber coxae – this is where a muscle attachment or its associated tendon or fascia has been damaged.
Small masses may also be palpated, which may be displaced bone chips. Small avulsion fractures have been observed in young racehorses, at the attachment of the Superficial gluteal muscle.
If there’s a pain response when you palpate these, bear in mind that it may be a sequestrum – ie. a bone fragment that has caused a lingering infection. This needs veterinary attention.
Alternatively, as Dr Sharon May-Davis explains (having examined fractures in dissections), these may also be ‘repair jobs’ that have happened as a result of bleeds. Smaller lentil-sized masses are calculi, ie. mineralized lumps, while the larger grape-like masses are lipomas, caused when a specialized fat is deposited in an effort to repair damaged tissue.

What are the lasting effects of a tuber coxae fracture?
If there are no further pelvic issues, the general view is that following recovery, the lasting effect of a tuber coxae fracture is little more than a cosmetic blemish.
Our study of 29 horses says that:
“The majority of horses in this study did have muscle atrophy or abnormal bony flattening over the affected tuber coxae. Horses with tuber coxae fractures have an excellent prognosis for returning to athletic use but will most likely have a permanent blemish associated with the area.” [1]
So, a couple of things here.
First, the horses in the study were sufficiently injured, ie. lame, for veterinary attention to be sought. This suggests the fractures were fairly severe, and it therefore follows that the fracture site would be noticeably different upon healing.
But second, what we don’t know about is the quality of the horses’ work post-recovery. They returned to their previous athletic work, but were they the same as before?
One lameness text states that this may only affect the careers of dressage horses, because they look asymmetrical, and judges may mark down due to this imprecision. [3]
Otherwise, the assumption tends to be that the localised trauma is no more than a superficial injury that leaves only a visual blemish, with occasional minor changes in gait quality.
As to whether horses are left with just that, quite a few people believe otherwise.
In fact, the rise of manual therapies has led to a lot more observation of gait changes and anomalies, such as those in the horse mentioned earlier.
Even while writing this, I went out and placed my hands on two more horses with this fracture and a noticeable effect on their movement.

The most affected muscles
Down to the nitty gritty – why my concern?
Let’s take a look at the effect on some significant muscles that have origins on the tuber coxae, and the related effect on movement if these attachments are damaged through the fracture.
-
Tensor fasciae late
The Tensor fasciae late muscle originates on the tuber coxae and the gluteal fascia. It has multiple insertion points, including (via fascial connections) the crest of the tibia bone and the lateral patellar ligament.
Its job involves flexing the hip, while extending the stifle (femeropatellar joint) as the hindlimb comes forwards.
It has a stabilising effect on the stifle through its connection to the patella ligament in front and the tibia.
This muscle does lose function when its attachment is permanently damaged. Even if it’s a small area of bone that’s lost up there, the effect lower down is broader.
-
Superficial gluteal
This muscle originates on the rear side of the tuber coxae (caudal) and the gluteal fascia.
It inserts onto the femur at the third trochanter. Its job is also to help flex the hip, while adducting the limb (bringing it inwards).
-
Internal abdominal oblique
The Internal abdominal oblique muscle originates from the tuber coxae and the inguinal ligament, and inserts onto the cartilages of the last 4 or 5 ribs, the linea alba, and the prepubic tendon.
Dr Sharon May-Davis writes that this muscle becomes overworked when engaged in supporting a hind limb lameness, and hypertonic when “excessively aiding pelvic engagement or [adopting] a supportive role in hind limb lameness.” [5]
[Biomechanical issues follow below.]

The biomechanical issues…
I’m sure you can see where this is heading now.
If muscles dedicated to flexing the hip suffer from impaired function due to a tuber coxae fracture, there’s going to be a negative effect on movement.
The horse can still move its hindlimb and flex the hip, of course, but an element of fine tuning is going to be lost. At least.
There’s also going to be compensation from other muscles, a functional asymmetry, and some stress in joints.
Generally speaking, the more bone that’s lost, the larger the negative effect on hindlimb control on that side.
Here’s what I’ve observed in various horses on the side affected by a tuber coxae fracture.
1. Outward rotation of the femur
The stifle is angled outwards, and the foot lands toe out.
The horse is less comfortable working in the same direction as the fracture, ie with the fractured tuber coxae on the inside of a circle. I’m presuming there’s a lack of stabilisation from the Tensor fasciae late and reduced function in this muscle.

2. Overdevelopment of the Rectus femoris muscle
This is the largest muscle of the quadriceps and the only one that attaches to the pelvis. It’s responsible for flexing the hip and extending the stifle. I presume this hypertrophy is due to compensatory action.
 3. Reduced function in the Superficial gluteal
3. Reduced function in the Superficial gluteal
This muscle is also responsible for flexing the hip. In cases with full tuber coxae fractures, this muscle is atrophied behind the point of hip, adding to the change in the outline of the hindquarters on that side.
4. Tension in the Iliacus muscle
Along with Psoas major, this muscle forms the Iliopsoas. I’ve presumed this tension from the positive responses to corrective moves for the Iliopsoas muscles on this side.
5. Lumbar imbalances
I’ve observed vertebral rotation and restriction, and painful tension in the caudal Longissimus dorsii muscles.
I assume this is due to the compensatory ‘swing and haul’ action required for protracting the hindlimb when there’s insufficient controlled flexion at hip level. Again, this would depend on the extent of the tuber coxae fracture.
Muscles that may also be directly affected
Depending on the anatomy of the individual horse, other muscles may also be affected. How much so depends on the extent of the fracture and the anatomical variations between individuals.
-
Iliacus muscle
Forming the Iliopsoas along with Psoas major, Iliacus is responsible for flexing and rotating the hip. It has an origin under the ilium and insertion on the lesser trochanter of the femur, along with the tendon of Psoas major.
-
Middle gluteal muscle
This massive muscle has multiple origins, including the ilium, and inserts onto the greater trochanter of the femur.
In some horses, the lateral edge of its origin on the ilium is close to the tuber coxae, and may be affected by a fracture. This major muscle is largely responsible for extending and abducting the hind limb (ie. moving it outwards, away from the body).
-
Accessory gluteal muscle
This smaller muscle is below the Middle gluteal, and works with it so closely that some texts describe it as part of the bigger muscle.
However, it is largely separate and has its own flat tendon that attaches to the greater trochanter of the femur. This insertion means that it also aids in abduction of the hind limb (ie. moves it outwards, away from the body).
Assessing the individual
In many cases, the apparently quick recovery from lameness can cause the horse’s owner to believe the fracture of a tuber coxae is of little consequence.
It may be true for some, but for others it may be more serious.
The only way to tell is to examine the horse as an individual, starting with a visual assessment and palpation with the hands, comparing one tuber coxae to the other.
The horse’s hind limb action should also be assessed for balance and evenness. The horse may not be lame, but may have limitations in its movement on the side of the fracture.
If muscles flexing the hip aren’t working as they should, other muscles may be compensating, and these in turn can lead to secondary pain.
If the effect on hindlimb action appears to be significant, it is worth considering veterinary imaging to measure the extent of the damage (although this can usually be felt).
At any rate, some rehabilitative work is probably going to be needed so that better muscle condition and strength can be developed on the fracture side.
Ultimately, in severe cases, we have to remember that ‘we can’t put back what’s gone’. This injury may well mean the horse is unsuited to certain sports.
But please, never assume that this is simply a cosmetic blemish.
References
[1] Dabareiner, R. M. and R. C. Cole (2009). Fractures of the tuber coxa of the ilium in horses: 29 cases (1996-2007). Journal of the American Veterinary Medical Association 234 10: 1303-1307.
[2] Pilsworth, R. C. (2003). Chapter 51 – Diagnosis and Management of Pelvic Fractures in the Thoroughbred Racehorse, Diagnosis and Management of Lameness in the Horse. M. W. Ross and S. J. Dyson. Saint Louis, W.B. Saunders: 484-490.
[3] Van Wessum, R. (2020). Lameness Associated with the Axial Skeleton. Adams and Stashak’s Lameness in Horses: 763-800.
[4] Ashdown, R. R.; Done, S. H.; Evans, S. A. (2000). Color Atlas of Veterinary Anatomy: Vol. 2: The Horse, 2nd ed. Mosby Elsevier: Edinburgh.
[5] May-Davis, S. (2023). Dissecting Out The Facts. Author’s workshop manual.


It is a pity that many of your references are so old. You only used two recent references the rest are old and considered out of date. I am sure you could have found recent references to back up what you are trying to say. References need to be within 10 years to be valid.
Thank you for your feedback. You are technically wrong on the point of references needing to be within 10 years to be valid. Using recent research is of course advisable, in instances where first, recent research exists, second, it builds on earlier research and third, it is good research. That is not the case here, as there is little coverage of the issue in research literature or popular texts. Nor was it the case in my equine PhD, where many references I used dated way further back as it was an under-researched area.
We were always taught to use approximately one reference per 200 words or two – four references per paragraph (point). This usually gave us at least ten references in a 2000-word paper, closer to 15. The only time I was permitted to use references older than ten years, was in a mini-systematic review. There were only six papers to review on my chosen topic, and I searched from 1935 to 2022. Once I had the papers, I had to find any similarities between those studies and then see if there were recent studies to verify the older data contained within them (where I could). I was very successful in my attempts. The university graded me well.
Great that you passed your units, but those guidelines do not relate to published scientific research or higher degrees by research for that matter.
Regardless, this is a blog post with a focus on helping horses with problems that are going unrecognised. I am astonished you felt compelled to comment as you did. Subject now closed.
Thank you for this blog. Not even the anatomy books are consistent on this matter and this explains many things to me and I have been a veterinarian for over 20 years. My personal horse, 4 years old QH has bilateral semi movable, snicker bar size lumps inches dorsal to the palpable tuber coxae. They are non-painful. When I ultrasound them, they are homogenous and look like the cross-section of any tendon. They have changed slightly in shape. She has body soundness issues. A tendency toward negative plantar angles, really drags feet, locked up SI, yet has the ability to flex and extend when you put her through a range of motion, but does not do it on her own. She does not tolerate circles or deep footing. She has what I believe are sciatic nerve fires when she canters sometimes. Hocks and stifles clean. Flexion tests negative…. So thank you, this blog gives me more to consider and I should not have ruled out fracture.
And thank YOU for this comment – I’m humbled that my writing has helped. I often question the wisdom of maintaining a blog that costs me to run, then something like this reminds me that it’s doing good out there.
As I was reading this, I was wishing there was some video showing what this might look like with a horse at a walk or trot. Also what symptoms to look for other the physical, like reluctance to move forward, aggression, those type of things? thanks Great post
Thank you for the feedback 🙂 I did take videos, but the results are more likely to mislead than to inform. Why? Because each horse is individual, in that they’ve other things going on too.
The best thing to do is palpate for the differences in the tuber coxae, identify a fracture (if there is one), and then take a good look at what’s happening with that particular horse – bearing in mind its other potential issues.
The most common change I’ve seen is the outward turn of the foot and leg, with medial placement of the foot in walk. Trot tends to obscure rather than expose these changes, as they’re not lamenesses and the elevation afforded in trot makes movement easier.
What a beautifully written account of this often missed condition. You clearly and succinctly highlight the need for further investigation of these cases and the need to include such fractures, and their effect on the horse, in equestrian education.
Thank you for this interesting article!
Well written and easily understandable for everybody.
Thank you for this feedback!
Thank you for casting light on this relatively undiscussed problem. I would just like to add my experience to the subject. My 23 y.o. PRE deleveloped a mystery lameness 2 years ago, 2 months after losing his stablemate, which mystified several vets. Eventually I found a coin-sized bald patch and, with palpation, a small piece of dislodged bone at the site of the tuber coxae. Unfortunately by this point he had been putting extra weight on his forehand for some time and, although his EMS had been under control for most of his life, developed laminitis so severe we almost lost him. Fortunately the specialist horse vet in our practice acted quickly and he recovered. He is now a healthy, happy retiree, unfortunately with PPID under control, but the laminitis angle is worth bearing in mind for EMS or potential susceptible horses.
Thank you for sharing your story. I’m sure that scenarios such as this mystery lameness are so much more common than recognized.
Another factor is that with these diagonal effects, it’s often hard to assess which direction the issue is travelling, and therefore source of the primary problem.
When the horse has an old tuber coxae injury and is affected by a fresh event elsewhere in the body, the compromised musculature becomes a renewed issue. I found a lot of pain in this area yesterday with a regular client who was presenting lame in the diagonal forelimb…